Focus areas
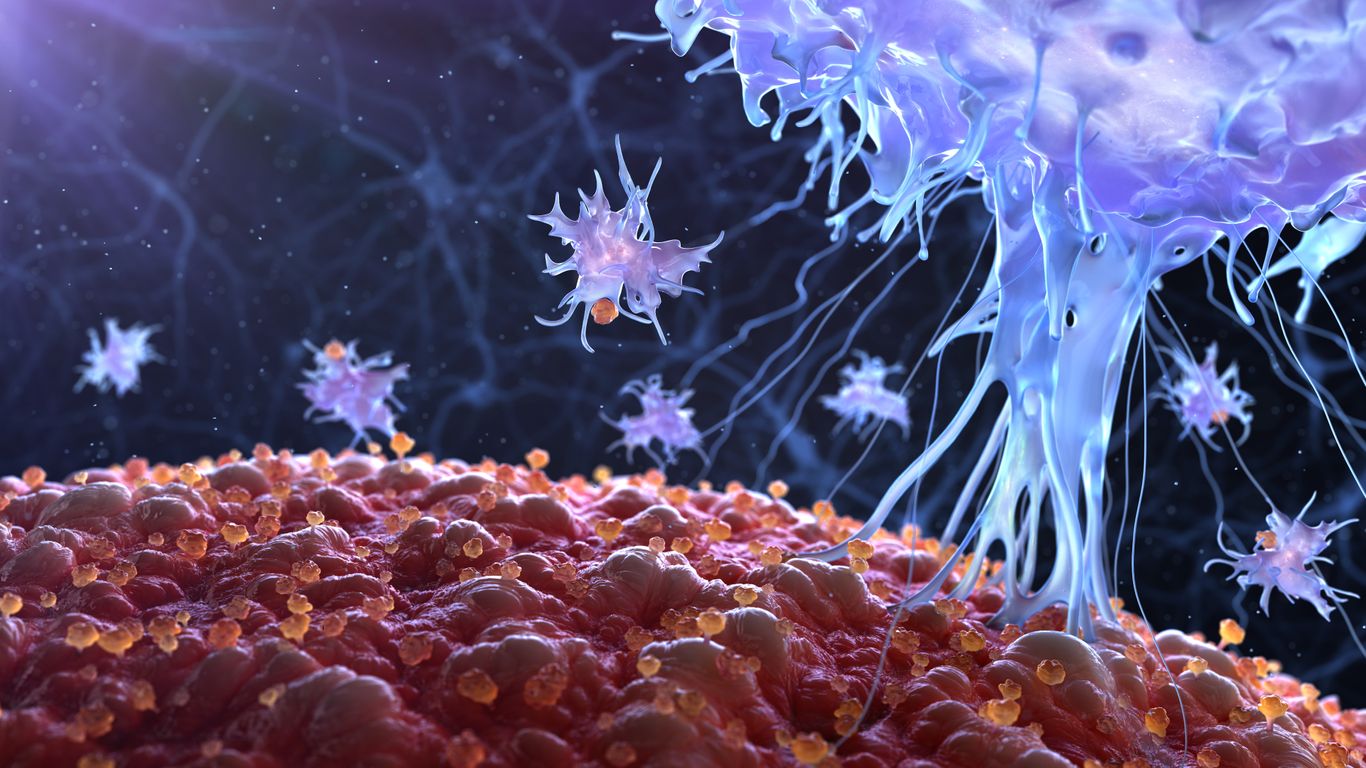
We develop innovative immunomodulating therapies with the potential to transform the lives of people affected by rare immunologic conditions.
Immunoglobulin G (IgG) antibodies constitute an important element of the protective immune response, but can, in some situations, be pathogenic or harmful.
By temporarily inactivating IgG antibodies, we aim to address conditions where IgG becomes harmful, including autoimmune conditions, or where the action of IgG antibodies interferes with the success of lifesaving gene therapies in rare disease or life altering procedures including transplantation.

Autoimmune diseases are caused by the immune system mistakenly mounting an attack against the body’s own cells and tissues often through the action of autoantibodies, antibodies that participate in the autoimmune attack.

It is estimated that currently up to 1 in 3 people may not be able to receive a gene therapy based on the use of Adeno Associated Viruses (AAV) due to antibodies that counteract the gene therapy treatment preventing its success.

Highly sensitized kidney transplant patients face extended time on transplant waiting lists due to a broad reactivity against human leukocyte antigens (HLA) that makes the identification of an immunologically suitable donor organ more difficult.